When you take paracetamol, it’s not the same paracetamol as the one I take. Well, it is - we pharmacists don’t have a special stash of drugs that we’re hiding from you. But our identical little white pills don’t necessarily have the same effect on everyone. We all respond differently to any drug, depending on a huge range of factors, like our age, gender, medical history, ethnicity and genetic make-up. Some drugs work perfectly for most people. For other patients, the drugs don’t work at all or, worse, cause side-effects that are more troublesome than the illness you’re trying to treat.
In an ideal world of ‘personalised medicine’, you’d give the right drug to the right person at the right time. And that’s where diagnostics come in: the ability to test patients accurately and quickly so you know exactly the best course of treatment.
For a simple headache (or hangover) we’re probably okay with one-size-fits-all paracetamol. It works just fine for most people, most of the time. But what about more serious problems, like cancer, HIV, heart disease - or Covid?
I’ve spent a lot of my career studying a particularly dangerous condition called sepsis. Latest estimates suggest sepsis affects around 49 million people a year worldwide. Of the 250,000 cases in the UK, up to 48,000 patients will die. It begins with an infection, which could be viral, bacterial or fungal. But sepsis isn’t the infection itself. It’s what happens when your immune system overreacts to the infection and starts to damage your body’s own tissues and organs. All too often, this over-reaction proves fatal.
Sepsis is a medical emergency, just like a heart attack, but it’s notoriously hard to diagnose. The symptoms are fairly non-descript, so early recognition is often difficult. Although the initial treatment is one-size-fits-all - antibiotics, oxygen and fluids – it’s really important that we administer these therapies as soon as possible in order to increase a person’s chance of survival. Every hour counts in sepsis.
This presents scientists like me with a challenge, and also an opportunity: to fix it. To think of better, quicker, and more accurate ways to diagnose an illness. To work out what’s causing it, and the best course of treatment for each individual case. And to monitor that treatment, hour by hour if needed, so clinicians know they’re on the right track.
Every illness leaves distinct ‘markers’ in a patient’s blood. Traditionally, you’d find the markers by taking a blood sample, popping it off to the lab, and waiting a couple of days for the result. Not an option with sepsis. You want a device that can accurately pick up all the clues simultaneously - sepsis has multiple markers - at the point-of-care, within minutes.
This is exactly the kind of problem I focused on during my PhD. Breakthroughs in the lab aren’t much use unless they’re helping patients out in the real world, so in 2014 we formed a company, Cotton Mouton Diagnostics (CMD) to provide a better solution.
We’ve developed a unique technology platform that can quickly detect markers for sepsis and other diseases like malaria, as well as screening people (and injectable medicines) for toxins from certain types of bacteria. Our devices are part of a much bigger picture: to fix big problems like sepsis, lots of different groups need to work together – us, clinicians, immunology experts, data-crunchers. It’s a huge collaborative effort.
Luckily, Wales is a really good place to get it done. Welsh Government, National Health Service (NHS) Wales and Welsh companies have embraced the concept of open innovation in Life Sciences. We recognise that we need to join forces to solve bigger problems. We’re a devolved nation, which gives us a nice discrete package of patients and a pool of data to work with. We’re also fortunate to be home to a number of research-intensive universities. Organisations like Life Sciences Hub Wales and MediWales pull everyone together.
At the risk of sounding immodest, we’re really good at it. We have 20% more Life Sciences businesses than the UK average, from start-ups to global blue-chips. The sector employs around 12,000 people in 360 companies and contributes £2bn to the Welsh economy.
There are obvious benefits to Wales itself: the more we innovate, the healthier (and wealthier) our population. But Welsh advances in digital and medical technology, regenerative medicine, diagnostics, pharmaceuticals and neuroscience extend beyond our borders to provide real differences to the lives of people all over the world.
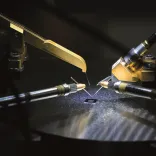
There’s a pipeline of innovation pouring through in Wales. You look at companies like Ortho Clinical Diagnostics, EKF Diagnostics and BBI Group who have helped pave the way in delivering point-of-care diagnostics. Creo Medical are doing great work in making tech for minimally invasive surgery, while Proton Partners International (now Rutherford Health) are pioneering advanced cancer therapies. There is also a steady stream of innovative and research taking place across our universities and within NHS Wales, which will ensure this rich pipeline continues to deliver for years to come.
The exciting thing is, you never know what discoveries will come next, and where they’ll lead. Medicine sometimes moves in mysterious ways. In 1993 a group of men in Merthyr Tydfil took part in a clinical trial of a little-known heart drug. They were the first men in the world to report unusual, and uplifting, side-effects. The drug rose to become a global sensation: Viagra.
To discuss opportunities in the Life Sciences sector contact us here